When to do a corticosteroid injection?
Injection with corticosteroids
By Dr. Jan Claeys, M.D.
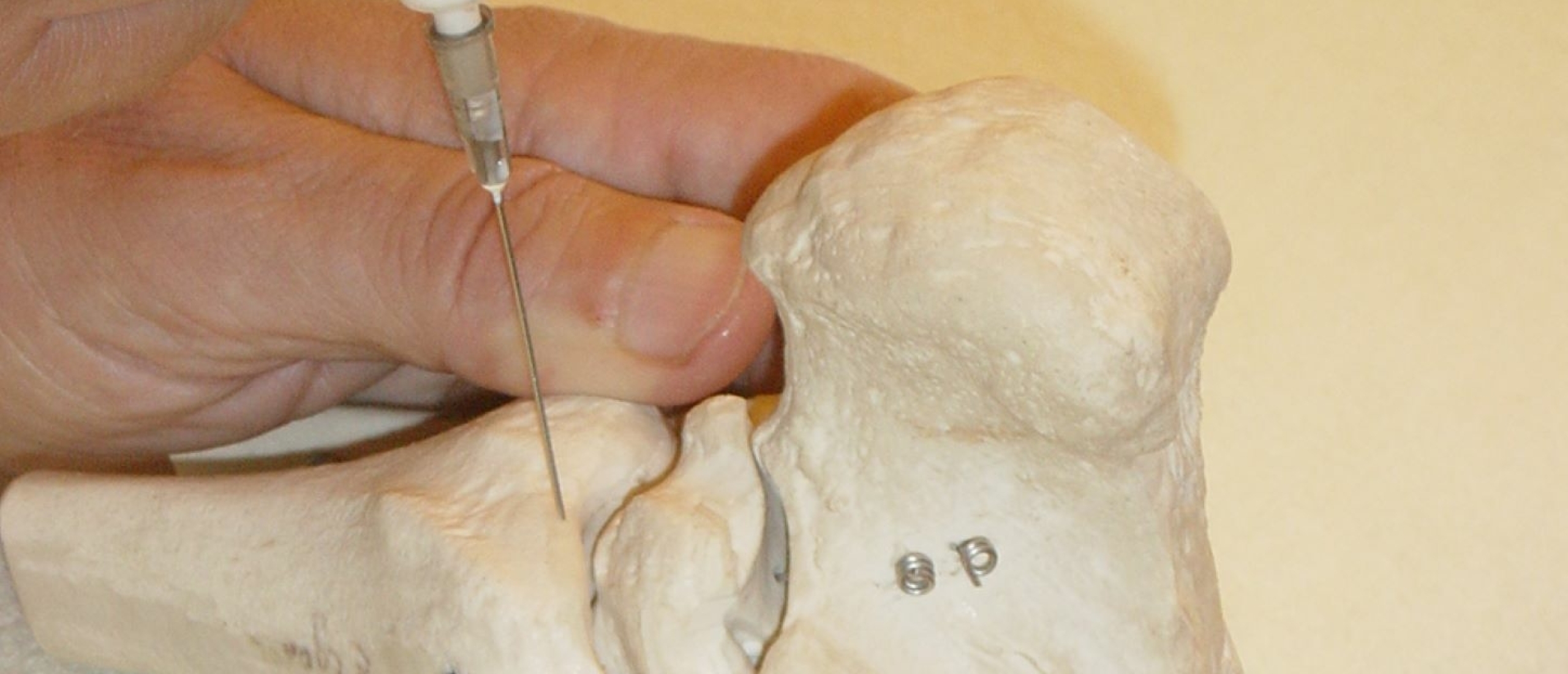
Indications of infiltration and injection techniques with corticosteroids
Corticosteroid injection, only in specific cases !
It is essential to inform the patient about the after-care, for fear of missing the expected therapeutic result.
After the use of triamcinolone acetonide in contractile structures the patient is asked to let the treated limb rest for a week, in order to get a maximal anti-inflammatory effect. The patient is re-examined after a fortnight and may need a second infiltration, again with the same indispensable after-care.
There is one exception to this rule : the treatment of a ligamentoperiosteal junction lesion by triamcinolone acetonide. From the next day onwards, active painfree movement of the joint, without actual exertion, should be encouraged in order to let the affected ligament move normally and thus avoid adhesion formation.
After an injection of triamcinolone acetonide into a joint the patient is asked, especially in weight-bearing joints, to avoid exertion of that joint in the next 24 hours.
As far as intra-articular steroid injections are concerned, it is generally agreed not to treat more than two joints simultaneously, with a maximal total dose of 50 mg triamcinolone acetonide. Usually 5 mg are used for small joints, 20 mg for average and 50 mg for hip and knee joints.
An interval of one month is a minimum for weight-bearing joints.
For steroid infiltrations in and around soft tissues, a second and a third infiltration are possible (in case of incomplete therapeutic result), each time with a fortnight's interval. In case of persistent failure, the diagnosis should be questioned or, if it proves correct, another therapy should be installed.
Possible benefits of steroid infiltrations or injections
Although the working mechanism of steroids has not yet been completely elucidated, a number of experimentally confirmed hypotheses exist, which can explain their anti-inflammatory action :
- Stabilization of the lysosomial membrane, with consequently a reduced release of lysosomial cytotoxic enzymes.
- Reduced formation of collagen and fibroblasts.
- Reduced formation of arachidon acid from fosfolipids with consequent reduced synthesis of prostaglandines
- Inhibition of the cellular metabolism of the inflammatory cells.
- Reduction of the synovial and capillar permeability.
Even when steroids are used locally, it is important to realize that there is still a temporary suppression of the hypothalamo-cortical axis, with a temporary reduction of the plasmacortisol .
Purpose of steroid infiltrations or injections
The ideal steroid answers the following three purposes :
- Little discomfort during and after the injection or infiltration.
- Prolonged topical effect, without local side-effects.
- Slight and slow absorption into general circulation.
The product that fulfils these conditions best is triamcinolone acetonide, mostly used in a concentration of 10 mg/ml. Using higher concentrations considerably increases the risk of side-effects.
Triamcinolone acetonide is a stable microcrystalline solution with an affect of about a fortnight.
Indications of steroid infiltrations or injections
The indications are either intra-articular or juxta-articular.
Intra-articular indications
The intra-articular application of steroids has a favourable effect upont the following disorders :
- Rheumatoid arthritis
- Arthritis occurring in gout or pseudo-gout
- Posttraumatic arthritis.
- Steroid-sensitive arthritis
- Psoriatic arthritis
- Arthritis in ankylosing spondylitis
- Arthritis complicating lupus erythematosus
- Synovitis of an osteoarthrotic joint.
Juxta-articular indications
Steroids have a beneficial effect upon the following disorders :
- Acute bursitis
- Lesions at the ligamento-periosteal insertion
- Lesions at the tenoperiosteal insertion
- Tenovaginitis and tenosynovitis
- Nerve compression disorders.
- Contraindications of steroid injections or infiltrations
- Contraindications can be absolute or relative ; in both cases due to local or general dangerous side-effects.
Absolute contraindications
Because of general dangerous side-effects :
- ill-defined diagnosis
- infectious arthritis
- bacterial endocarditis
- in case of coagulation disturbance
- immune deficiency diseases (leukemia, aids, ...).
Because of a local dangerous side-effect :
- major local skin infection
- joint prosthesis
- joint with osteochondral fracture.
Relative contraindications
Because of general dangerous side-effects :
- diabetes patient with insuline dependency
- former tuberculosis.
Because of a local dangerous side-effect :
- at an unstable joint
- haemarthrosis
- decubitus sulcusin case of coagulant therapy with coumarines and heparines.
Side effects of steroid infiltrations and injections
Most side-effects are usually reversible ; they are rare in case of a precise diagnosis, with an accurate injection or infiltration technique and a scrupulous respect of the general directives.
- Steroid arthropathy
Intra-articular steroids can be responsible for cartilaginous degeneration. The more injections, the greater the possibility of this degeneration.
In an intra-articular injection, the tip of the needle can cause a minor tear in the cartilage ; if repeated, this cartilage damaging can be the cause of a chronic osteoarthritis.
In case of repeated injections, particularly at the hip, aseptic necrosis can ensue.
- Crystalline synovitis
Crystalline synovitis appears a couple of hours after the injection and abates within 1-3 days. Too fast an intra-articular application is thought to be a predisposing factor.
Patients who get intra-articular steroids should be informed about this side-effect.
- Local skin atrophy and depigmentation
These side-effects are thought to be due to leakage of the steroid solution into the derma when withdrawing the needle. These lesions are usually reversible, but recovery can take months.
- Tendinous ruptures
To avoid these serious side-effects, infiltrations are only possible along the tendon, between tendon and tendon-sheath or at the tenoperiosteal junction. Moreover, the number of infiltrations should be kept as low as possible.
- Local granulomatous lesions
Microcrystalline deposits in the soft tissues can in certain cases cause the formation of, at times painful, local granulomas.
- Septic arthritis
This dangerous side-effect is usually caused by poor asepsis. Diabetes patients and patients with immune suppression are here particularly vulnerable.
- General allergic reaction
This appears generally a few minutes after the injection or infiltration and disappears mostly spontaneously within a few hours or days.
- Very exceptionally an anaphylactic shock can occur.
- Uterine haemorrhage
This occurs only on repeated steroid injections or infiltrations. Steroids do not seem to have any teratogenous effect.
- Peripheral nerve damage
This damage is caused by the intrafascicular effect of the steroid and by direct traumatic effect of the needle. The symptoms are severe pain and dysesthesia, together with motor deficit in the territory of the nerve. The damage can be permanent.
- Systemic side-effects
These occur only if the maximal dose per application or the maximal number of applications is exceeded. In such case, the hypothalamo-cortical axis is suppressed with, as a rare consequence, adrenal gland insufficiency. Glycaemic deregulation and osteoporosis can also occur.
