
Shoulder functional examination
What does the specific shoulder history learns us?
When the patient suffers from a tendinitis/tendinosis, then the history will provide us some basic information. In case of an arthritis however, then the history becomes much more important.
It will help us to determine which kind of arthritis it is (traumatic ?,…) and will also reveal the stage of the arthritis. How acute or chronic is it?
This is very important information since the treatment strategy in each stage is quite different.
We ask the standard questions :
- what is the problem,
- where are the symptoms felt,
- since when did it start,
- how did it start,
- how did it evaluate,
- how can you influence the symptoms (for better and worse),…
Focus more specifically on following questions:
1. Where is the pain : local pain or referred problem ?
Are the patient’s symptoms the result of a local lesion or is the pain referred from e.g. the cervical spine ?
Remember that shoulder structures have a C5-origin and thus will refer pain somewhere in the C5-dermatome. The AC-joint will refer pain in the C4-dermatome.
Of course the specific history will mostly provide you enough information to decide if it is a shoulder or a cervical problem.
(in case there is any doubt: also check some cervical functional tests and see whether or not you can provoke the patient’s symptoms by doing those tests).
2. Was there any injury or overuse ?
A capsular pattern found after injury or overuse most likely suggests a traumatic arthritis. Keep in mind other types of arthritis do exist.
3. What is your age ?
A traumatic arthritis apparently does not occur under the age of 40-45 y. This is a purely empirical finding for which we don’t have solid scientific proof yet.
4. When did it start ?
It’s not only interesting to know whether the lesion is acute or chronic.
Some lesions also have a spontaneous evolution, and that might have a consequence on the therapy level:
Example :
- an acute subdeltoid bursitis recovers in about 6 weeks, the first 3 weeks are, without treatment, a real “horror”.
- A traumatic arthritis recovers in about 1 year.
Depeding on in which phase of the spontaneous evolution the lesion is, the treatment will be different. (I refer to other chapters for more details).
5. Are there any other joints affected ?
If so, then we have to consider disorders such as rheumatoid arthritis., psoriatic, lupus erythematosus,…
6. Did you ever have surgery ?
If the patient had a breast surgery e.g. 3 years ago and now she/he presents with a shoulder problem, then be aware of inherent unlikelyhoods.
The following three questions are very important to determine the stage of an arthritis :
- Can you lie on that side at night ?
- Is there any pain at rest ?
- Is there any radiation of pain below the elbow ?
Stage I arthritis :
This is an arthritis “light”.
There is a favourable answer on the three questions :
- Yes, I can lie on that side,
- no pain at rest,
- no radiation below the elbow.
Stage III arthritis :
This is an acute arthritis.
There is a non-favourable answer on the three questions :
- No, I can’t lie on that side,
- I have pain at rest,
- there is radiation below the elbow.
Stage II arthritis :
- II minus : two favourable answers, one unfavourable.
- II plus : two unfavourable answers, one favourable.
Depending on the stage, the treatment procedure will be different.
Functional examination
Sometimes symptoms in the shoulder area are referred from the cervical spine.
If necessary, we perform a preliminary cervical examination for differential diagnostic purposes.
If cervical tests cleary influence the patient’s symptoms then we have a positive link and we perform the complete cervical examination. If cervical tests are negative, we proceed with the shoulder examination.
The challenge is to collect as much information as possible by using as less tests as possible. There is no need for excessive testing. If necessary, some complementary tests (see film below) may be useful.
All tests need to be performed bilaterally.
Active elevation
 Active elevation
Active elevation
We assess pain and range of motion (ROM). Although this test does not enable us to differentiate between a lesion of an inert or a contractile structure, it gives us a good idea of the patient’s willingness to move.
This is not a glenohumeral test but rather an aspecific shoulder girdle test.
We distinguish three components :
- some 90° of glenohumeral abduction,
- 60° rotation of the scapula along the thorax (serratus anterior and upper trapezius muscles ; possibly involved in a mononeuritis of the long thoracic nerve)
- and 30° of glenohumeral adduction (pectoralis major muscle ; possibly involved in a mononeuritis of the spinal accessory nerve). These three components do not occur strictly successively.
Beware of some inherent unlikelihoods :
even with a completely ankylosed shoulder joint, when muscles and nerves function normally, there still has to be some 60° of arm elevation, due to the intact scapular rotation.
Also keep in mind that the range on passive elevation is always bigger than that on passive glenohumeral abduction.
Passive elevation
 Passive elevation
Passive elevation
We assess pain, ROM and end-feel (elastic).
Grasp the elbow, not the forearm, for a more precise execution of the test.
If the shoulder is quite mobile, ask the patient to perform an active neck flexion to create some space for the movement.
Painful arc
 Looking for a painful arc
Looking for a painful arc
Ask the patient to do an elevation movement, slowly, and he has to tell us what he feels, where and when.
We may not miss a painful arc in the shoulder, since mostly this is an important localizing sign.
So, we are looking for a painful movement section, inbetween two painfree sections.
Indicating something is squeezed in between humerus and acromion. (more details will be discussed in another chapter).
If the arc is so severe that the patient is unable to lift his arm beyond the horizontal without help of the other arm (i.e. a passive painful arc), severe calcification in a tendon or a bursa is suspected. This is an empirical finding.
Passive glenohumeral abduction
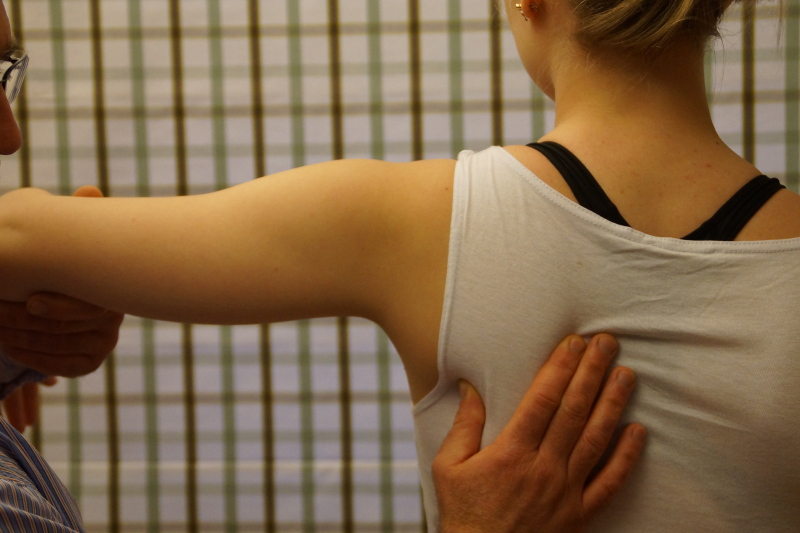 Passive glenohumeral abduction
Passive glenohumeral abduction
The thumb fixes the inferior angle of the scapula, the arm is raised passively untill we feel the end of movement. The scapula remains fixed. We assess the ROM (normally 90°).
Passive lateral rotation
 Passive lateral rotation
Passive lateral rotation
We assess pain, ROM and end-feel (elastic).
Make sure to block the heterolateral shoulder, so that the patient cannot do a compensatory movement, and sometimes (when the patient is very mobile) the therapist has to step slightly backwards to reach the real end of range.
This is important, since some lesions only cause end range pain.
In case of an arthritis, keep following detail in mind:
Stage III arthritis :
The lateral rotation movement will be quite painful resulting in a limitation with muscle spasm end feel due to increasing pain.
Stage I arthritis :
There will be limitation of ROM too, but only end range pain ; so, first we will find the limitation and when giving slight overpressure we will provoke some pain.
Passive medial rotation
 Passive medial rotation
Passive medial rotation
It is important to stabilize the patient’s arm, to prevent an improper execution of the test (we have to focus on medial rotation instead of retroflexion). We assess pain, ROM and end-feel (elastic).
A painful arc on medial rotation is possible, so, don’t stop the test movement too early! If it is painful, ask the patient where the pain is felt and try to continue the movement, allowing us to discover a possible painful arc.
A painful arc on medial rotation very often suggests the presence of a chronic subdeltoid bursitis.
The normal range on medial rotation is 90°. How do we assess a limitation ?
- The movement stops at the patient’s trousers pocket (-30°)
- at the back pocket (-15°)
- at the sacrum (-5°).
At this point in the examination we distinguish between a capsular and a non-capsular pattern.
Capsular pattern = limitation lateral rotation > abduction > medial rotation.
Note: the limitation of movement can be variable, but the ROM proportions between these three movements are important.
Resisted adduction
 Resisted adduction
Resisted adduction
We test : teres minor, maior, latissimus dorsi and pectoralis maior.
Resisted abduction
 Resisted abduction
Resisted abduction
We test the supraspinatus and deltoid.
Resisted lateral rotation
 Resisted lateral rotation
Resisted lateral rotation
We test the infraspinatus and teres minor.
Note the counter pressure at the patient’s heterolateral shoulder and the resistance given proximal from the wrist.
We ask the patient to do a lateral rotation, and perhaps it is useful to first show the patient what exactly we mean.
Our experience shows that many patients perform an abduction rather than a lateral rotation, which again endangers the final diagnosis.
Resisted medial rotation
 Resisted medial rotation
Resisted medial rotation
We test the subscapularis, teres maior, pectoralis maior and latissimus dorsi.
Resisted elbow flexion
 Resisted elbow flexion
Resisted elbow flexion
We focus on the biceps muscle.
Resisted elbow extension
 Resisted elbow extension
Resisted elbow extension
We focus on the triceps muscle.
Keep in mind that during a resisted test, inert structures may be compressed :
e.g. a resisted extension can compress an inflamed subdeltoid bursa, thus provoking pain into the C5-dermatome.
Accessory tests
Passive horizontal adduction
 Passive horizontal adduction
Passive horizontal adduction
This test can be positive in three particular cases :
- acromioclavicular lesion
- subscapularis tendinitis
- subcoracoid bursitis.
More accessory tests (e.g. in relation to mononeuritis) are illustrated in the film below.
Accessory functional examination in relation to subacromial impingement
An extensive overview of so-called impingement tests and it’s interpretation is illustrated in the powerpoint podcast below.
